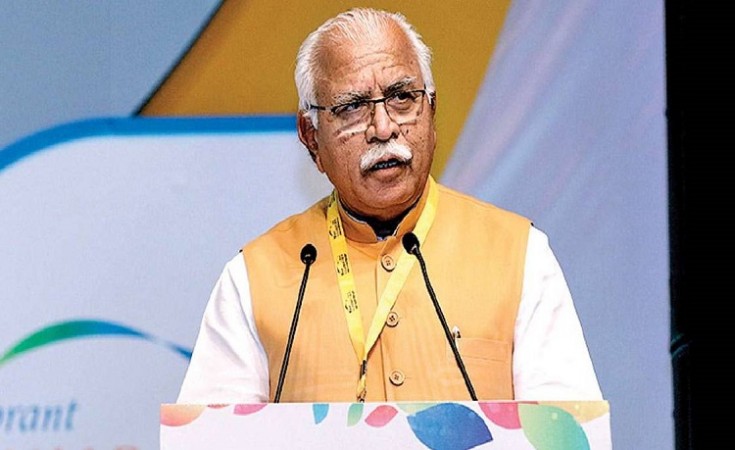
Haryana: In a bid to amplify its focus on the social sector in the current fiscal year, the Chief Minister of Haryana, Manohar Lal Khattar, announced on Saturday the extension of the Ayushman Bharat scheme's benefits to families with an annual income ranging from Rs. 1,80,000 to Rs. 3,00,000.
As per an official statement released by the Haryana Chief Minister's Office (CMO), families falling within this income bracket will be able to access the advantages of the Ayushman Bharat scheme by submitting a deposit of Rs. 1,500. The registration portal for this purpose is set to go live from August 15, according to reports.
While already 30 lakh families have been benefiting from the Ayushman Yojana, an additional eight lakh families will now become eligible, as highlighted in the statement.
It's noteworthy that the preceding year witnessed the government led by Manohar Lal Khattar raising the annual income threshold for inclusion in the scheme from Rs. 1.20 lakh to Rs. 1.80 lakh for Below Poverty Line (BPL) families.
The Ayushman Bharat scheme, aimed at providing healthcare coverage to all BPL families, facilitates free medical services up to Rs. 5 lakh. The state currently boasts 715 empaneled hospitals operating under this scheme.
Meanwhile, media reports surfaced on August 10, revealing serious irregularities in the Ayushman Bharat scheme in Madhya Pradesh, as discovered in a nationwide audit conducted by the Comptroller and Auditor General of India (CAG).
The audit found that approximately Rs. 1.1 crore had been disbursed to around 403 patients who were erroneously listed as 'deceased' in the database. Moreover, the report noted that across the state, nearly 8,000 patients were shown to be simultaneously admitted to multiple hospitals during the same period.
Within the report, the CAG identified 24 state-run hospitals, including a government facility, that reported significantly higher occupancy rates than their actual bed capacities.
The audit also highlighted instances where 25 hospitals submitted claims for 81 patients twice, pertaining to various surgical treatments. Notably, the Madhya Pradesh health authority processed full payments for both claims, contrary to the stipulated rate of 50% payment for the second claim.
To date, over 23 crore beneficiaries have undergone verification and have been issued Ayushman cards, enabling them to avail themselves of cost-free medical treatment under this scheme.
National Health Authority Launches 100 Microsites Project
Mandaviya Launches 2nd Phase of Nationwide Mass Drug Admin Campaign